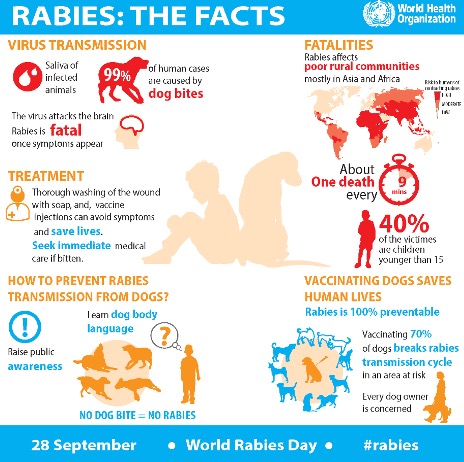
Everyone has heard of rabies. It strikes fear into people, with and without pet dogs. It is one of the oldest know diseases in the world, yet there is still no cure for it. Read on to find out more about the disease that claims the lives of almost 60,000 people each year across the globe.
You can also find out what Manali Strays does to help combat rabies in Kullu District, India
Rabies in Animals
What is it?
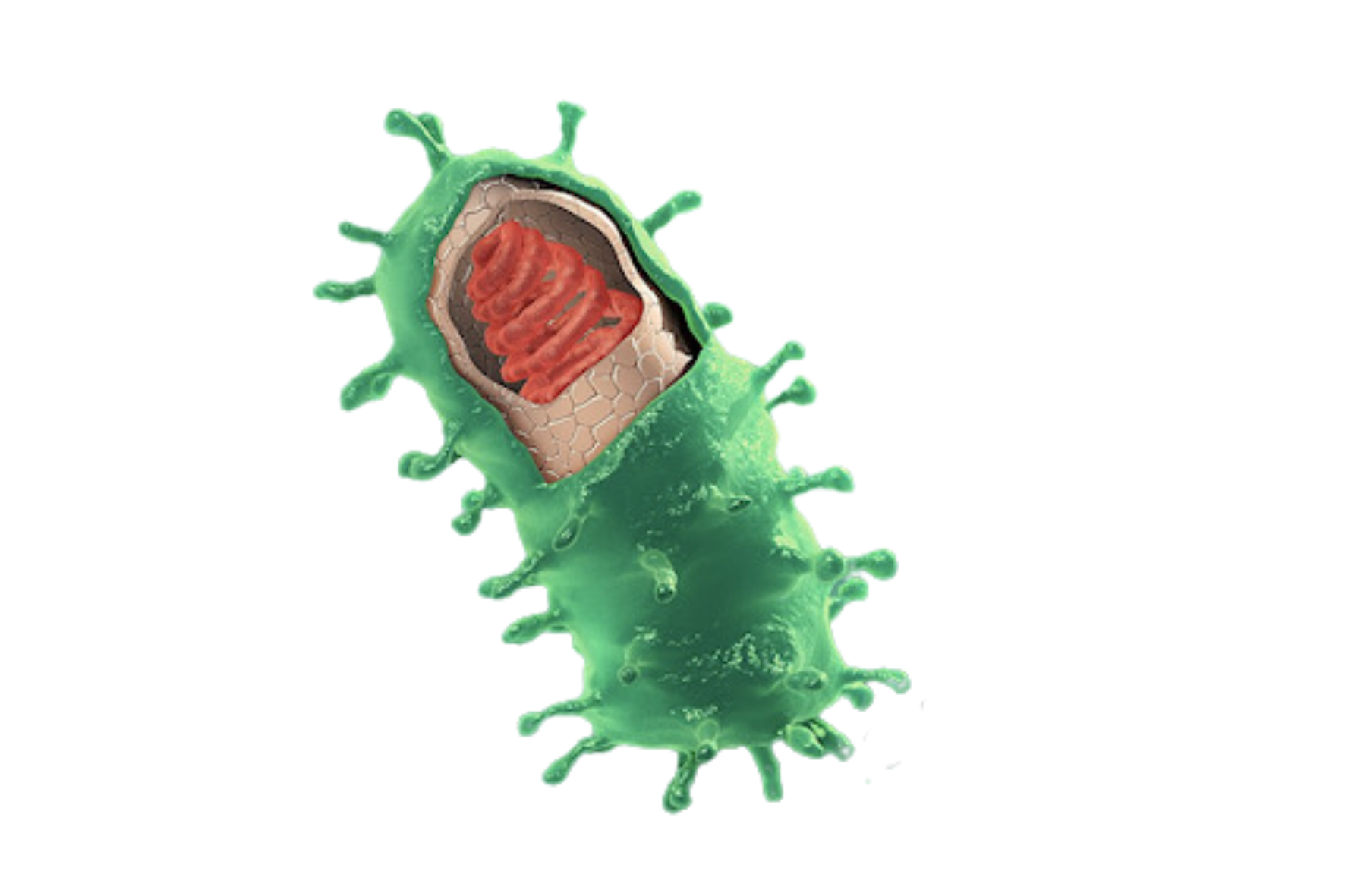
Rabies is a zoonotic disease, meaning it can spread from animals to people. It is caused by the rabies virus, and is fatal once symptoms develop… in animals and people. The disease has been around for centuries, with references to it dating back to the 18th century BC.
The virus infects nerve cells causing encephalitis (brain inflammation) and eventually death.
How is rabies transmitted?
Animals primarily become infected with the rabies virus when saliva carrying the virus enters the body via the bite of an infected animal, usually a dog or bat.
On rarer occasions, licking of a wound or scratching (infected saliva can be on the claws from the animal licking its paws) can allow the virus to be transmitted.
Once the virus has entered the body, it usually replicates in muscle cells initially, before moving to nerve cells. The virus spreads via the nerves from the site of initial infection to the brain. After exposure, symptoms do not manifest until the virus has reached the brain (incubation period), which varies greatly, ranging from days to months, or even years. Generally, the farther the bite is away from the head, the longer it takes for the virus to reach the brain and for symptoms to develop. Other factors affecting the incubation period include the amount of virus transmitted and the severity of the wound. In dogs, the incubation period is usually two to 16 weeks. After reaching the brain, the virus infects the salivary glands where it can then be passed on to other animals via biting.
When the virus is in the salivary glands and being excreted into the saliva it is known as “shedding”. In dogs, shedding can start three to six days before any symptoms manifest, during which time they can transmit the virus to other animals if they bite. For this reason, if a dog bites another animal or person and you do not know whether or not it has rabies, it is recommended to isolate and observe the animal for 10 days. If after 10 days it is not showing signs of rabies, it can be concluded that the biting animal did not have rabies.
What are the symptoms of rabies?
As with many of these diseases, individual symptoms are non-specific and can be signs of other medical problems. However, there are some signs that can be indicative of rabies. There are three phases, commonly known as “prodromal phase”, “furious phase”, and “dumb phase”. Infected animals can go from the furious to the dumb phase or only exhibit one of these phases.
Prodromal Phase: this is the first phase and may go unnoticed as it only lasts for 2 or 3 days. Signs include:
- Behavioural changes – friendly dogs may start to nip or bite and normally aggressive dogs may become friendly and affectionate
- Anxiety
- Irritability
- Seeking solitude
- Fever
- Licking/scratching at the bite wound – the site of the bite can become quite itchy.
Furious form: This is the classical type, and is actually less common in dogs and cats despite popular culture usually depicting rabies as causing “mad dog” syndrome. Signs include:
- Abnormal behaviour
- Aggression
- Excessive salivation due to paralysis of the throat and jaw muscles
- Biting at objects such as rocks and moving items.
- Restlessness
- Hypersensitive to visual and noise stimuli
- Seizures
Paralytic form: Also known as “dumb” rabies, this type is the most common form seen in dogs and cats and occurs when the rabies virus infects and destroys motor neurons. The first muscles to become paralysed are usually the throat and jaw, causing salivation. The paralysis progresses to include the diaphragm, and the legs. Signs include:
- Excess salivation
- Lower jaw hanging open
- Gagging as though something is lodged in their throat.
- Laboured breathing – deep shallow breathing
- Inability to stand/walk
A dog that Manali Strays was called out to, in the paralytic stage of rabies; unable to stand, laboured breathing, and his lower jaw has dropped down due to paralysis of the jaw muscles.
How is rabies treated?
Sadly, once the virus has reached the brain and symptoms start there is no treatment, and humane euthanasia is the recommended action. Rabies is a painful disease, and although the animal will die on its own, it is extremely inhumane to leave the animal to die slowly over several days. That being said, anybody coming across an animal suspected of having rabies should always contact an organization equipped to deal with it safely and humanely.

How is infection prevented?
Of course the answer is vaccination
The first vaccine should be given at three months of age. It is recommended to give a booster one month later to ensure that the dog develops a proper immune response that will last until its yearly booster. One study showed that dogs given only one vaccine did not have a high enough antibody titre one year later to confer immunity. Whereas those that received the booster one month later had a much better immune response.
Additionally, if a dog is ill with a fever, or a condition like demodectic mange, it means that their immune system may not work well enough to produce a proper response. In these cases the dog may experience vaccine failure, so always make sure your dog is healthy when it is first vaccinated.
Puppies/kittens:
- 1st Vaccine – 3 months old
- Booster – 4 weeks later
- Then yearly boosters.
Dogs & cats over 6 months old:
- 1st vaccine – as soon as possible.
- Then yearly boosters.
Rabies in humans
As rabies can also affect people, we are including a section on vaccinations for humans.
Like in animals, it is fatal once symptoms begin. Although, a few people have been cured using a very intensive treatment that involves being placed in a chemically induced coma.
There are three vaccination protocols: pre-exposure prophylaxis, post-exposure prophylaxis for previously vaccinated individuals, and post-exposure prophylaxis for unvaccinated individuals.
Regardless of your vaccination status, if you are bitten by a potentially rabid animal you should carry out the following immediately:
Wash with soap, detergent, or povidone-iodine solution under running water for at least 15 minutes. This is to flush out and kill as much of the virus as possible, reducing the amount that can enter the cells and begin traveling to the brain.
Pre-exposure Prophylaxis
This is a course of three vaccines in the arm muscle and means you don’t need to have immunoglobulin, if later bitten. This is ideal if in a high risk environment or in a location where access to immunoglobulin is limited.
Vaccine Schedule:
- Day 0 – anti-rabies vaccine
- Day 7 – anti-rabies vaccine
- Day 21 or 28 – anti-rabies vaccine
Post-exposure prophylaxis for individuals previously vaccinated
If you have already had rabies vaccines and are then bitten by a potentially rabid animal, you should receive two vaccines in the arm muscle. The vaccine acts as a booster to kick start your immune system into producing antibodies very quickly. These antibodies then neutralize the virus before it reaches the brain.
Vaccine Schedule:
- Day 0 – anti-rabies vaccine
- Day 3 – anti-rabies vaccine
Post-exposure prophylaxis for individuals never vaccinated
If you have never received any rabies vaccines and are bitten by a potentially rabid animal, you should receive rabies immunoglobulin (antibody) at the site of the wound plus four rabies vaccines in the arm muscle. Rabies immunoglobulin is injected into the site of the wound (usually a bite) and acts by neutralizing as much of the virus as possible. This reduces the amount of virus that can enter the body and travel to the brain. In the meantime, rabies vaccine is also given to make your immune system produce its own antibodies against the virus, but this takes time; approximately 7 to 10 days.
Vaccine Schedule:
- Day 0 – Immunoglobulin at the wound site + anti-rabies vaccine
- Day 3 – anti-rabies vaccine
- Day 7 – anti-rabies vaccine
- Day 14 – anti-rabies vaccine